Cerebral Palsy is an ‘umbrella term’ that results from injury to the developing brain in the first few years of life (during pregnancy or shortly after birth). It is the most common condition that causes physical disability in childhood. The impact cerebral palsy has on a child can range from very mild to very severe.
here can be many different causes of cerebral palsy that can occur during pregnancy, around or after the birth of a baby .Multiple births and premature births are more well-known risks, but many other factors can cause cerebral palsy (e.g .genetic factors, infections). It is sometimes possible to find the reason why a child has cerebral palsy, while in other cases a direct cause cannot be identified.
Adjusting to a new diagnosis
No matter your situation, it is common for parents to feel a great sense of loss following the diagnosis. Grief is expressed in many ways and it can affect every part of your life; your emotions, thoughts and behaviour, beliefs, physical health, sense of self and identity and your relationships with others. Grief can leave you feeling sad, angry, anxious, shocked, regretful, relieved, overwhelmed, isolated, irritable or numb.
Grief has no set pattern and everyone experiences it differently. Some people may grieve for weeks and months, while others may experience grief for much longer. You may also find that your grief is reactivated as your child progresses, or is slower to progress through different developmental stages. Through the process of grief, you will begin to create a new relationship with your child that accommodates those feelings of loss, but which leaves room for hope and a positive outlook.
It is important for you to know that all of these feelings are common and you may find that it is helpful to discuss these feelings with your family members and those involved in the care of your child. You may also seek out the support of a qualified health professional, who is trained to provide psychological intervention which assists in understanding and processing your grief. There is always support available so please ask for this if you feel it would be helpful.
How is Cerebral Palsy Diagnosed.
History: a detailed birth and developmental history.
Examination: this may include a clinical neurological examination, as well as video recordings of your child’s
movements, which can be carried out by a trained professional (usually a GP, Paediatrician, Rehabilitation Specialist or Allied Health professional).
a. The recommended clinical neurological examination is called the ‘Hammersmith Infant Neurological Examination’(HINE) which is useful for infants between 2 and24 months corrected age.
b.‘ General Movements’ (GMs) are assessed through video recordings of your child between birth and 3 months ’corrected age. Typical and non-typical movements can be recognized and assist with identifying infants ‘at risk’ of cerebral palsy. You may be able to video your child’s ‘General Movements’ at home through an App called ‘Baby Moves’. Your therapist will discuss this with you if relevant.
Investigations: these can include a cerebral ultrasound, MRI brain and blood tests.
Ultrasounds are an easy and non-invasive test which can be performed on infants in their first few months of life when their so� spot (anterior fontanelle) is still open.
Magnetic Resonance Imaging (MRI) of the brain can also be done as a ‘Feed and Wrap’ study in a special incubator designed for premature small babies. However, as babies grow and develop, sedation is required to ensure
no movement occurs at all during their brain MRI. It is recommended that all infants with cerebral palsy have a repeat brain MRI at age two once their brains are fully developed. Children aged five and above may be able to lie still for their MRI. At the Queensland Children’s Hospital, we use a practice MRI to assess whether these children require a general anaesthetic.
c. Sometimes, other investigations need to be carried out, such as investigating genetic or metabolic causes of a child’s condition. These are usually blood tests, some of which can take a few months before results are available. Urine tests may also be requested and you will be shown how to collect these from your child.
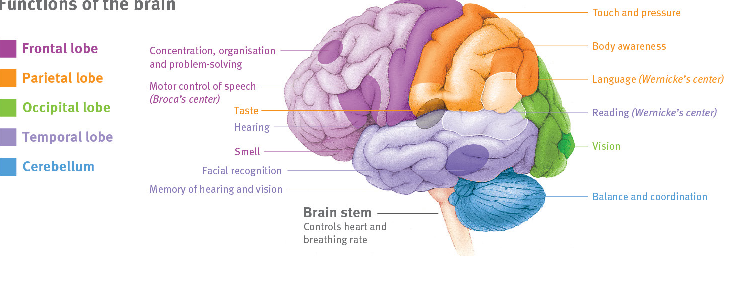
Types of cerebral palsy
Cerebral palsy is described according to the type of movements (motor type), as well as the area/s of the body affected (distribution). You may see these terms written on documentation about your child (e.g. clinic letters).The most common motor types seen in cerebral palsy include:
1.Spastic:This is the most common motor type. It describes‘ stiffness’ in muscles which worsens with speed and
movement. The faster you move a child’s limb, the more stiffness or resistance to that movement you will feel. It may also increase when the child is excited, sad or scared (extremes of emotion), or when he/she is trying really hard with an activity.
2. Dyskinetic: Movements are altered and involuntary, with the main types being:
Dystonia –This describes movements which have sustained or intermittent muscle contractions which
cause abnormal postures, repetitive and/or twisting movements. A child’s muscles may fluctuate between being floppy and stiff and will be relaxed when asleep.
Athetosis –Movements are slower, more continuous and look like a writhing action.
Chorea –Movements are often random and ongoing, appearing in smaller fragments.
3.Ataxic: Children with ataxia are often more floppy and have difficulty with their balance and orienting their body in space. Tremors (shaky movements) are common.
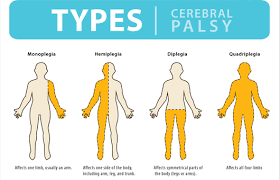
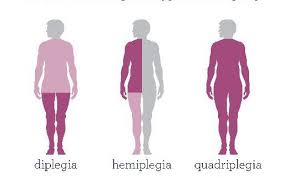
Which body parts are affected?
Cerebral palsy can affect various parts of the body and each child presents differently. Common terms you may come across include:
Quadriplegia/bilateral (quad=four):Both arms and legs are affected, usually also involving the child’s
trunk.
Diplegia/bilateral (di=two):Both legs are affected.A child’s arms may also be affected, but to a lesser
extent than their legs.
Hemiplegia/ unilateral (hemi= half):Only one sideof the child’s body is affected (one arm, one leg).

 June 05, 2025 - BY Admin
June 05, 2025 - BY Admin